
Japan’s Eighth COVID Wave: A Closer Look at Case Numbers and the Hospital Crisis
February 7, 2023
R-2022-078E
Amid continuing reports about rising numbers of COVID-19 cases in Japan, the government revised the Infectious Diseases Control Act on December 2, 2022. The amended law aims to secure sufficient numbers of hospital beds and bolster access to outpatient medical care, but will the changes be enough to address the hospital crisis? Are existing COVID policies reasonable in the light of the available evidence? Are we on the cusp of achieving herd immunity? And do we have a true grasp of the number of people infected? Members of the research program on Establishing Health System Resilience to Tackle the Health Security Crisis sat down to discuss these and other issues with a close look at the data.
Fluctuating Levels of Immunity
TOSHIKAZU KUNIYA: As of November 27, the cumulative number of COVID-19 cases in Japan has surpassed 24 million.[1] In order to predict future trends, our research team used the SEIR [susceptible-exposed-infectious-recovered] mathematical model to estimate herd immunity levels in several major prefectures in Japan and published the results in a previous article on this website [in Japanese].
Herd immunity levels temporarily increased during the sixth and seventh waves in Japan but are now falling. Due to the sharp decline in vaccine-derived immunity levels, it’s essential that we promote additional vaccinations to prepare for future outbreaks, especially for those who have yet to be infected.[2]
KENJI SHIBUYA: Epidemic waves occur when the level of herd immunity derived from vaccines and natural infection declines, and cycles of vaccination and natural infection may be something we’ll have to adapt to as the “new normal.” The article you mentioned was published at the end of October, and the estimates made then have largely materialized, with infections rising again in what can be called the eighth wave.
Do Reported Case Numbers Tell the Whole Story?
KIYOSU TANIGUCHI: Figures announced by the Ministry of Health, Labor, and Welfare also show a clear increase in the number of infections.[3] There are problems, though, with the way these numbers are counted. As an example, let’s take a look at the number of newly infected cases reported by medical institutions in Mie Prefecture.
Figure 1. COVID-19 Infections in Mie Prefecture (through November 7, 2022)
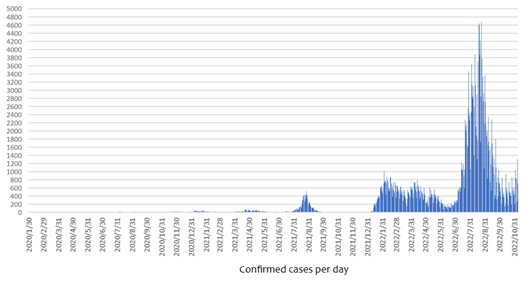
Source: COVID-19 infection trends in Mie Prefecture, https://www.pref.mie.lg.jp/YAKUMUS/HP/m0068000066_00002.htm.
COVID-19 cases are based on physicians’ reports, but if people don’t experience symptoms, they’re not likely to go to a clinic or hospital, and asymptomatic cases will be underreported. As the number of infections with mild symptoms increases, it will become more difficult to identify surges based solely on reported cases.
The following figure shows five years of influenza notification data from Australia. At a glance, it would appear that the number of cases were highest in 2022.
Figure 2. Influenza Notifications in Australia, 2017–22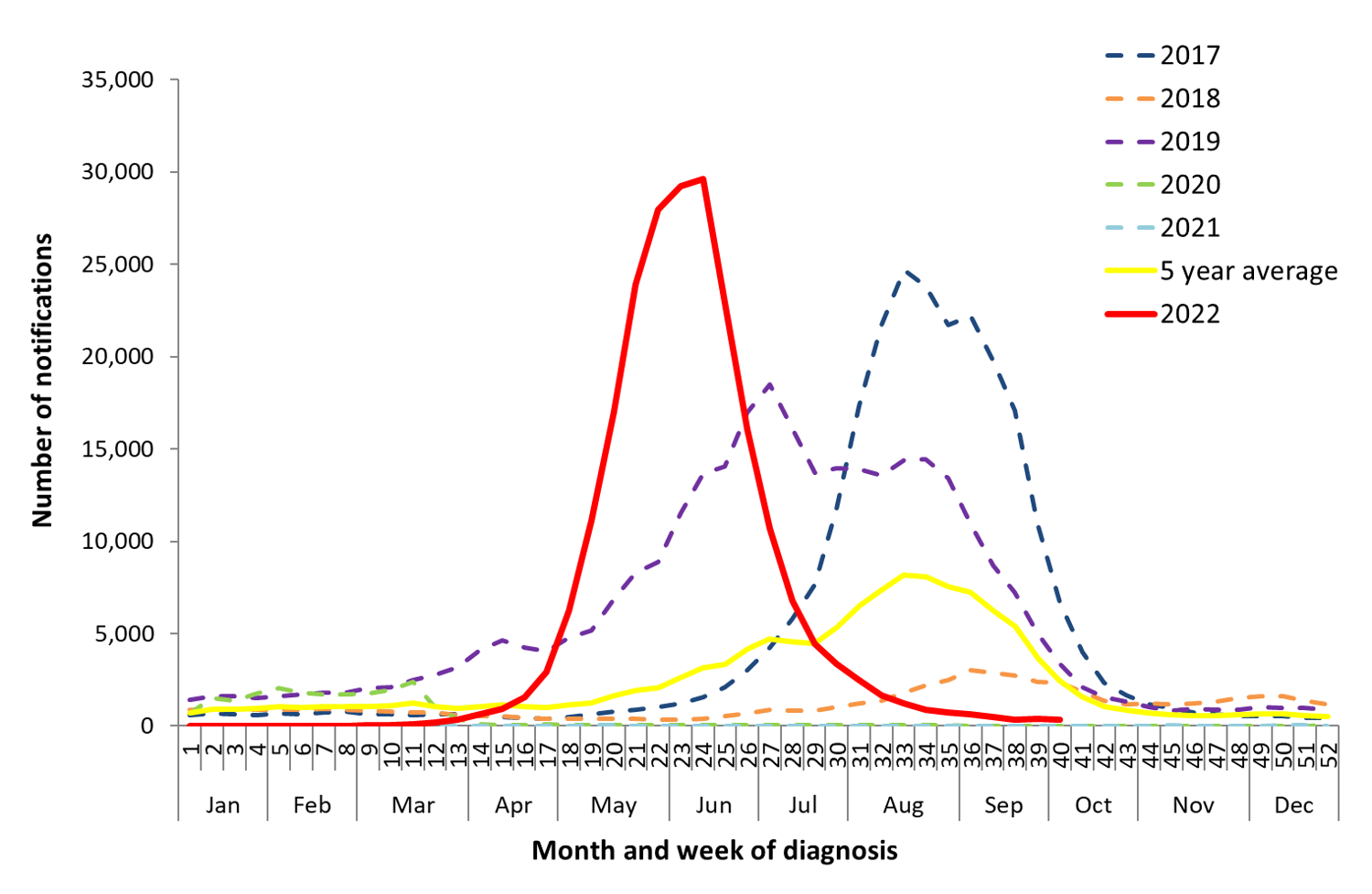
Notifications of lab-confirmed influenza, Australia, 01 January 2017 to 09 October 2022, Australian Influenza Surveillance Report, https: //www.health.gov.au/resources/collections/aisr
However, surveillance of influenza-like illness—which causes symptoms of fever and acute respiratory illness—tells a different story. The numbers of ILI patients per 1,000 consultations in 2022 are not very different from the five-year average. Here, the much higher rate for 2017 is the outlier.
Figure 3. Influenza-Like Illness Rate per 1,000 Consultations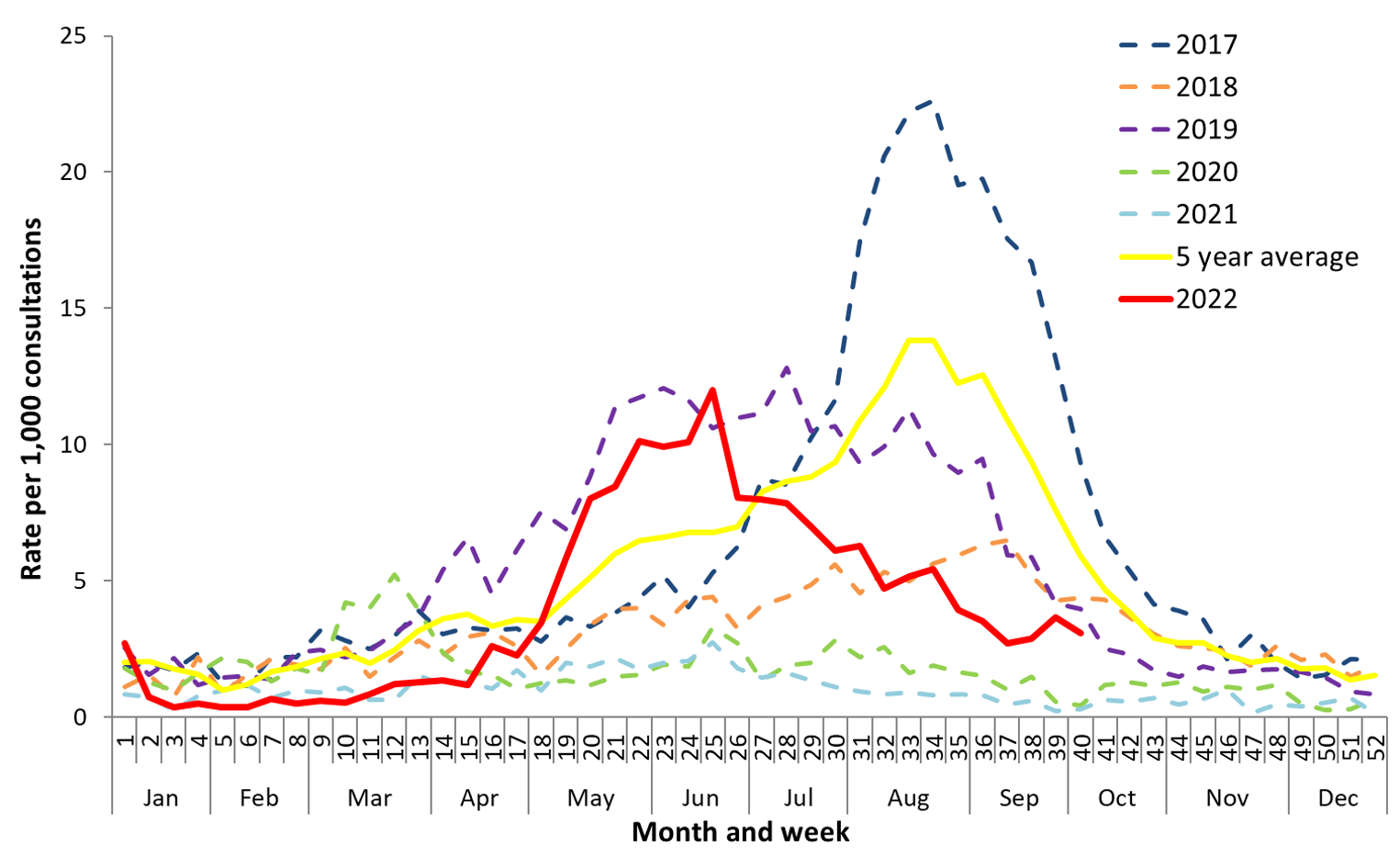
Unweighted rate of ILI reported from ASPREN sentinel GP surveillance systems, Australian Influenza Surveillance Report, https://www.health.gov.au/resources/collections/aisr.
Australia’s positive rate for influenza in winter 2022 was 15 percent, about half of previous outbreaks, which generally had positive rates above 30 percent. Based on this data, the Australian government stated that the impact of influenza in 2022 was mild to moderate. The notification numbers are not compatible with the real situation, as they are affected by consultation behavior and testing policy in clinics.
Figure 4. WHO Influenza Report for Australia, November 2022
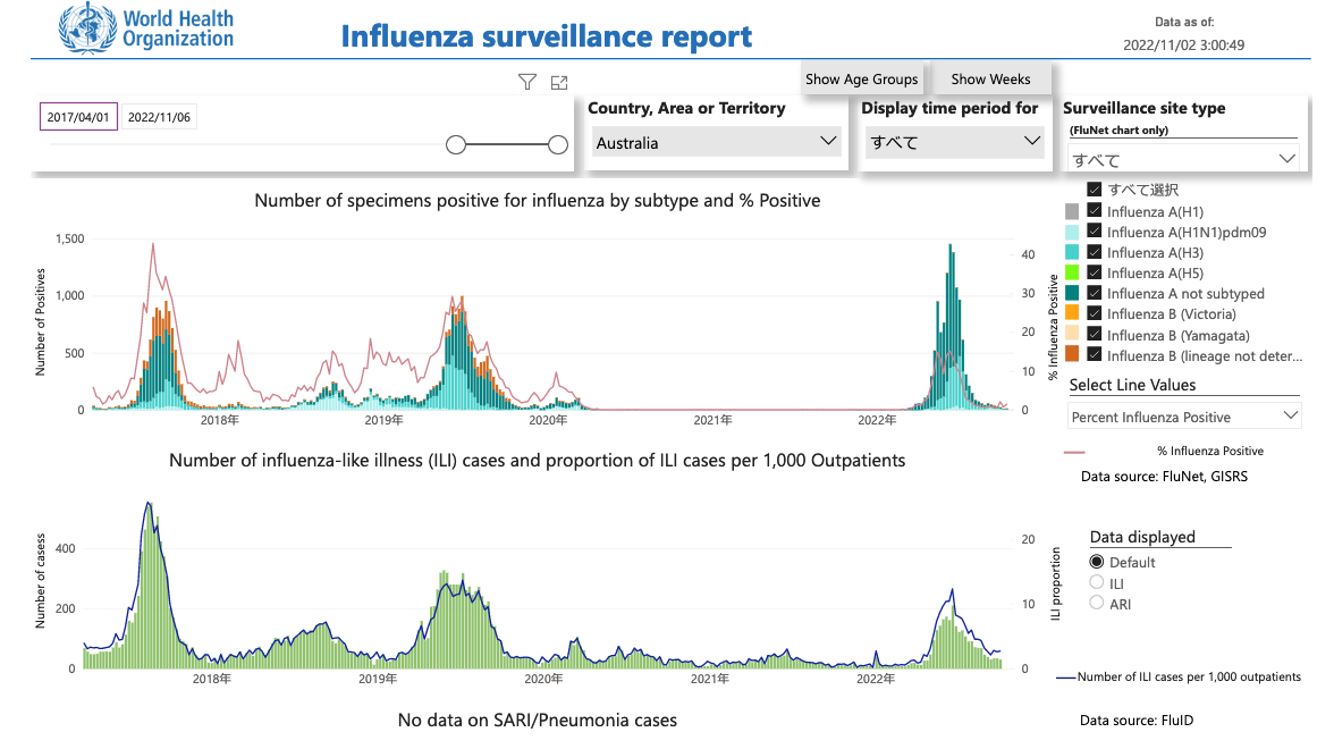
WHO Global Influenza Surveillance and Response System (GISRS) https://app.powerbi.com/view?r=eyJrIjoiYWU4YjUyN2YtMDBkOC00MGI1LTlhN2UtZGE5NThjY2E1ZThhIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9.
Figure 5 is the ILI surveillance data for Mie Prefecture. During the week of October 31 to November 6, the influenza positive rate was 0.63 percent, suggesting that even if you had a fever or other ILI symptoms, the risk of actually having the flu was very low. The positive rate for COVID-19 among patients with symptoms was 24.38 percent, however. In other words, the likelihood of a positive test result for someone with symptoms was less than 1 percent for influenza but around 25 percent for COVID. With such data, it’s easier to get an overall picture of the epidemic, and physicians can predict the risk of COVID in patients who come to the hospital with a fever. Looking at positive test cases in relation to the total number of patients with influenza-like symptoms will help us better assess epidemic conditions and the true burden of health-care facilities by the number of patients who actually show up .
Figure 5. ILI Surveillance Data for Mie Prefecture, Oct 31–Nov 6, 2022 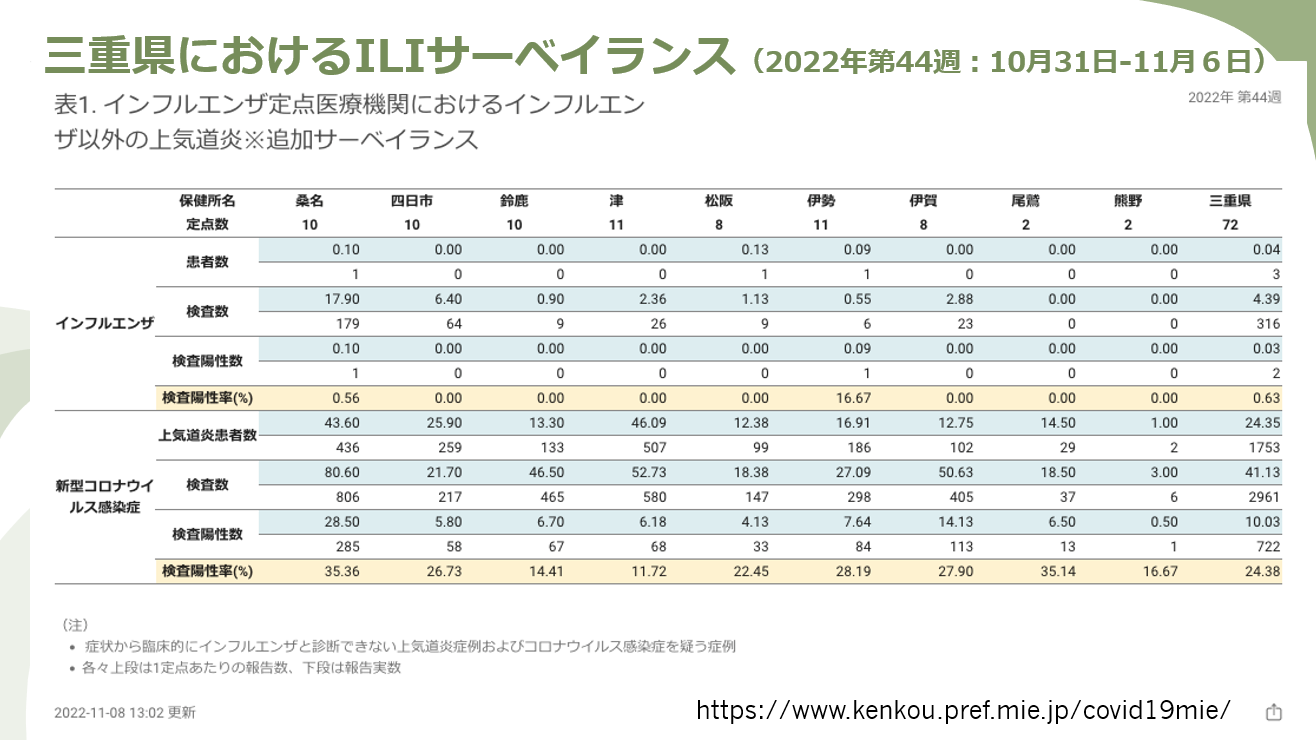
SHIBUYA: We’ve learned that conducting sentinel surveillance at medical institutions is very important. On the other hand, properly diagnosing patients and conducting surveillance requires a well-functioning health-care system. What should be done to prevent the system from breaking down?
Hospital Staffing Shortages
YASUHARU TOKUDA: Many people have puzzled over how a crisis in Japan’s health-care system could occur when some 900,000 acute care beds are available. According to data from August 2021, only around 40,000 of these beds—or about 5 percent—were being used to hospitalize patients requiring urgent care. Comparable data from the United States shows the figure was over 20 percent. Simply put, the problem wasn’t the number of beds but a shortage of health-care professionals. Until the end of the outbreak of the Delta variant, COVID patients received care in the ICU. With the emergence of the Omicron variant, however, hospitals have been focusing on treating exacerbations of baseline diseases under general care, especially as many patients have partial immunity.
This makes the residency system an important factor. Residents are recent medical school graduates who rotate through various departments during the course of their training and gain experience in general care. Since quickly increasing the number of physicians can be difficult, making more effective use of residents can be key to overcoming the shortage in medical staff.
As we adapt to the new normal that involves living with the coronavirus, I think it’s essential that we rebuild our health-care system with consideration for both quality and quantity. We need to increase the number of doctors over the long term, but in the interim, we should set up a system capable of dealing with the pandemic with the existing number of physicians and other health professionals, including those at private and community hospitals.
TANIGUCHI: When people hear about a hospital crisis in Japan, they immediately think in terms of the number of beds, but we ought to be thinking instead about the staffing shortage. A strained health-care system means potentially losing lives that could be saved, as ambulances carrying COVID patients are unable to reach to hospitals with available care. In this situation, we have to reduce the number of infections in the community in order to allocate enough hospital care to critical cases.
Surviving the Eighth Wave
TANIGUCHI: As for influenza, existing measures are probably enough to prevent it from becoming a major epidemic. But with COVID, Japan doesn’t t yet have enough people with hybrid immunity, compared to Europe and the United States, given the smaller number of people who were naturally infected. The challenge, then, will be to raise the level of immunity largely through vaccination. As the number of mild cases increases, though, fewer people will go to the hospital, and this will make it harder to determine the community transmission level based on reported numbers alone.
SHIBUYA: Do you think movement restriction will become necessary?
TANIGUCHI: It’s possible that the number of infections could increase quite rapidly if more people move freely. Most cases will be mild, though, and we won’t need to shut down the economy, but steps should be taken to make sure that hospitals have enough capacity to treat patients with more severe symptoms by transferring mild cases to primary care physicians.
Ever since the Omicron variant became dominant, the rate of people developing severe symptoms has been declining. That being said, the condition of certain high-risk patients can still deteriorate quickly. Small children are also at high risk for severe cases, so we might need to bolster pediatric care. As for movement restrictions, they may not be needed if people have a good understanding of infection-prevention measures and if adequate health-care enhancements can be made.
SHIBUYA: Dr. Kuniya’s predictive model shows Okinawa Prefecture maintaining a high level of herd immunity.
KUNIYA: This was derived from natural infection, similar to urban areas like Tokyo and Osaka. On the other hand, Hokkaido’s immunity is derived more from vaccination than infection. Looking at the number of reported cases through November 8, it appears that the eighth wave arrived early in Hokkaido, while it will be slow in coming in Okinawa.
A Medical System for the New Normal
TOKUDA: The number of infected people in Okinawa has been increasing since the second week of November, but as of November 11, Okinawa had the fewest cases per capita among prefectures in the Kyushu region. Inpatients occupied only 12 percent of COVID beds, so there’s still plenty of room. There are questions, though, about whether we have enough surge capacity. For example, to reduce the rate of hospitalization, the antiviral drug Paxlovid must be administered to high-risk patients within five days of getting sick, but if the primary care system is shut out of treating COVID patients, they won’t be able to benefit from this drug at all.
Reducing hospitalization requires more testing, early diagnosis, and the administering of drugs to high-risk patients. And when hospitalization does become necessary, we need to expand the type of institutions accepting patients to include smaller, community hospitals, not just specialized facilities like regional medical care support hospitals and advanced treatment hospitals. Likewise, infectious disease specialists need not be the only health-care professionals treating COVID patients. Greater use should be made of other available human resources. We also need to improve the testing system for medical staff and shorten their quarantine period when infected. In short, we need a well-thought-out strategy to cope with epidemics.
TANIGUCHI: Prior to COVID, almost all medical facilities were able to treat patients with fever during the flu season. Given that early diagnosis and treatment are especially important for high-risk patients, the limitations on the institutions able to treat COVID could result in a vicious cycle of delayed diagnosis and more severe cases. It’s absolutely essential that smaller, local hospitals be able to treat fever patients.
SHIBUYA: Since the Omicron variant is so contagious, hospitals could easily become overwhelmed if there’s a jump in cases. I feel the key is to maintain hybrid immunity through natural infection and vaccination.
TANIGUCHI: The immunity derived from vaccines diminishes over time and doesn’t offer sufficient mucosal immunity. Evidence is emerging that hybrid immunity offers the best protection, but when people are infected without having been vaccinated, there’s a danger that they may develop severe symptoms and suffer from lingering aftereffects, commonly known as long COVID. So it’s important that vaccines come first, before natural infection. With vaccination and then natural infection, severe cases could gradually be decreased.
SHIBUYA: To sum up our discussion, preventing a health-care crisis requires controlling outbreaks initially through vaccines and allowing more medical institutions to treat COVID patients, which will obviate the need to enforce movement restrictions. We also need to make more informed assessments of epidemic conditions by conducting probabilistic surveillance, rather than by just looking at the number of reported daily cases.
We have to coordinate better, keeping an eye on herd immunity levels, ascertaining trends through surveillance, and optimizing the health-care system for our new normal of living with COVID. Recent amendments to the Infectious Diseases Control Act introduced penalties for advanced treatment hospitals that fail to secure enough COVID beds, but playing the blame game isn’t very constructive. I have a feeling that people aren’t willing to put up with movement restrictions much longer, so there’s a greater need for data-based policies that truly match the reality on the ground. (Compiled by Kana Masuda)
Translated from an article originally published in Japanese on December 2, 2022; slightly abridged.
[1] Ministry of Health, Labor, and Welfare, “Visualizing the Data: Information on COVID-19 Infections,” accessed November 27, 2022, https://covid19.mhlw.go.jp/extensions/public/en/index.html.
[2] The model used captures changes in herd immunity levels by taking into account the effects of immunity attenuation over time. However, it does not account for reinfection, immune escape, behavior change, or transient collective immunity (changes in individuals’ social behaviors over time).
[3] Ministry of Health, Labor, and Welfare, “Shingata korona wirusu kansensho no kokunai hassei doko” (Trends in Domestic Outbreaks of COVID-19 Infections), accessed November 3, 2022, https://www.mhlw.go.jp/content/10906000/001008673.pdf.
![]()
Subscribe to the Tokyo Foundation for Policy Research eNewsletter.













