Web 3.0 and the Future of Health Care
November 14, 2022
In his presentation at the July 22 symposium hosted by the Tokyo Foundation for Policy Research, Kenji Shibuya highlights the systemic failures in Japan’s health-care sector and advocates transitioning to more a decentralized approach to develop trust and enable people to take control of their own health.
* * *
Digital transformation is sweeping through the health-care sector, encouraged by proposals in the Cabinet Office’s 2022 basic economic and fiscal policy guidelines to establish a national medical information platform, standardize electronic medical record information, apply digital technologies to the revision of medical service fees, and establish a medical DX promotion headquarters. The World EXPO Osaka, Kansai, scheduled for 2025, will include demonstrations of surgical procedures aided by augmented reality and physical rehabilitation incorporating virtual reality.
But these cannot really be called examples of a digital transformation. The Oxford dictionary defines transformation as “a complete change in something.” Because none of the above initiatives will lead to a “complete change,” they would be better described as attempts at digitization. Given that systemic failures in Japan’s health-care sector were glaringly exposed by the COVID-19 pandemic, digital technology will need to be fully harnessed to achieve a transformation in the true sense of the word. Doing so will require, as I argue below, ending our myopic preoccupation with reducing health-care spending and making a radical shift toward a health-care system that operates much like a decentralized autonomous organization (DAO).
Are Health-Care Expenditures Really Too High?
The pandemic has revealed some of the long-neglected vulnerabilities of Japan’s health-care system. Ever since last summer’s fifth wave of COVID infections, people have been left to die at home because hospital beds were unavailable. This came as a shock to many in Japan, a country that prides itself on universal health coverage meant to ensure that everyone can receive appropriate and affordable medical care when they need it. Because an overwhelming majority of hospitals in Japan are privately run, with most offering a wide range of nonspecialist services, it is no surprise that they struggled to cope with the surge in demand for specialized medical care during the pandemic.
The government is fully aware of these issues, though. In July 2020, the Liberal Democratic Party’s Headquarters for the Promotion of Administrative Reform, chaired by Yasuhisa Shiozaki, proposed a fundamental revision of the Infectious Diseases Control Law, first enacted more than 120 years ago. This was a landmark proposal that pushed for changes in the public health system centered on the National Institute of Infectious Diseases and the country’s network of public health centers. The proposal was ultimately watered down, however, and the administrative divide between the systems for public health and medical care was left intact. As a result, the current health-care system is heading toward collapse. The time is now, as COVID-19 transitions from a pandemic to an endemic, to transform—that is, to completely change—the country’s health-care system.
While everyone agrees on the need for social security reform, most discussions zero in on controlling health-care costs. The pandemic has revealed the inadequacies Japan’s health-care system and sent government subsidies soaring. It is understandable, then, that many have jumped to the conclusion that the medical establishment has reaped big profits from the pandemic and that health-care expenditures should be slashed. The fact of the matter is, though, that people who have been fighting for the lives of COVID patients are totally exhausted. This is partly due to the fact that the number of beds to accommodate such patients, notably at acute-care public hospitals belonging the National Hospital Organization or Japan Community Healthcare Organization, accounted for just 5% of the national total during Japan’s severe fifth wave. Rushing to cut medical expenditures without first analyzing the conditions within the health-care system risks further aggravating the dysfunctions in the system, pushing an already struggling system to the brink.
The dominant opinion among government officials in the Ministry of Finance and elsewhere, along with many health economists, is that health-care expenditures must be cut. They reason that spiraling medical and nursing-care costs from an aging population account for the bulk of social security expenditures, which have now climbed to tens of trillions of yen. But if we look at the data more carefully, we can see that this is not only short-sighted but can also be counterproductive.
An international comparison of social security benefits as a percentage of GDP in relation to the aging rate shows that although Japan’s population is aging rapidly, there has not been a concomitant rise in social security benefits in relation to GDP. Figure 1 shows that Japan’s population is aging far more quickly than other countries, but this is due not so much to an increase in the number of elderly than it is to a fast-declining birth rate. The population of those 75 years or older is increasing gradually and will eventually peak out, but the working-age population is shrinking because there are fewer births. The basic problem, then, is not that a growing elderly population is pushing up Japan’s social security expenditures but that there are fewer working people paying into the system.
Figure 1. An International Comparison of Social Security Benefits (as a Percentage of GDP) in Relation to the Aging Rate, 1980–2015
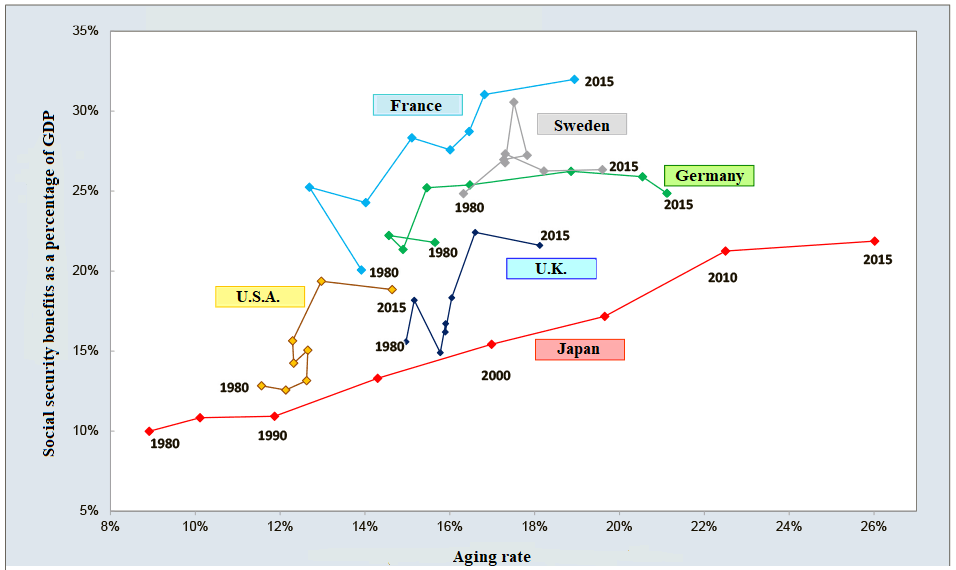
Source: Ministry of Health, Labor, and Welfare.
Social security projections published by the Ministry of Health, Labor, and Welfare (MHLW) shows health care and nursing care as the two main areas where costs are expected to soar. But many earlier projections of future medical expenditures have proven to be overestimates. This is only to be expected, though, since the aim of such forecasts is not to accurately predict the future but to undertake scenario analysis of potential developments and explore policy options. Estimates of medical expenditures will be significantly influenced by policy interventions and assumptions made by the model used for such estimates, as can be gleaned from the widely disparate projections of COVID-19 cases.
For important issues, a fairer basis for policy debate would be to use estimates published by independent think tanks, rather than by the government ministries in charge of those policies. For example, Hosei University Professor Kazumasa Oguro has projected that medical expenditures will likely decrease in the future (Figure 2). We need to keep in mind that population aging is due mainly to a declining birth rate and that rising health-care costs can largely be explained by new but more expensive medical technology, rather than the swelling ranks of senior citizens.
Figure 2. Long-Term Trends in Nominal Medical Expenditures (¥ trillion)
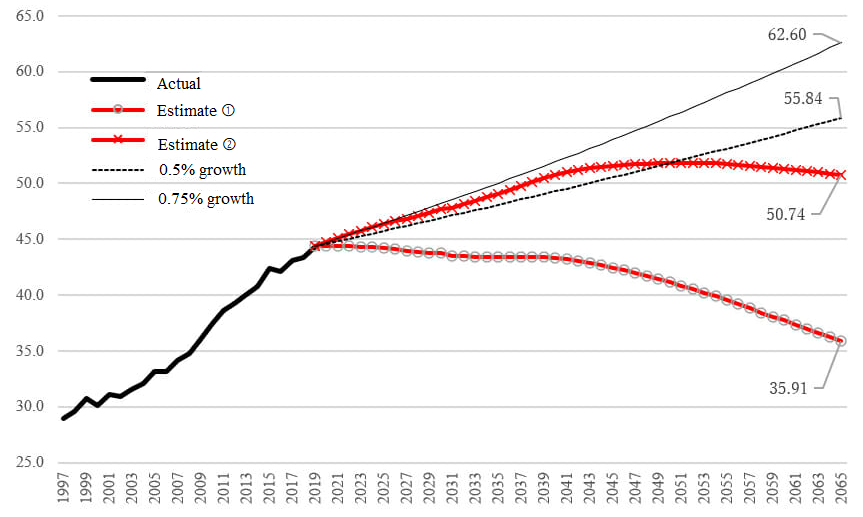
Source: Kazumasa Oguro (https://cigs.canon/article/20220413_6710.html).
An attempt to reduce medical costs by targeting a natural, biological process is surely missing the forest for the trees. If we agree that the health-care system provides us with great added value, then we should be prepared to pay a commensurate price for it. At the same time, the desire among fiscal authorities to prevent medical outlays as a percentage of GDP from spiraling out of control is understandable. But this is an unfounded concern. A far more constructive way of keeping a lid on rising expenditures would be for the medical community come up with a plan to keep medical costs down to around 10% of GDP. We can then move beyond the myopic focus on equating aging with higher costs.
Overworked Young Physicians
Will the pressure to keep spending down have an impact on health-care standards in Japan? The World Health Report 2000, published by the World Health Organization, contains an international comparison of health-care system performance as of 1997. As one of the report’s authors, I recall feeling proud of the fact that Japan ranked first in that survey. The data available to us was quite limited at the time, however. Of the WHO’s 193 member states, only around one-third—mostly developed and middle-income countries—published usable data. For most developing countries, we had to rely on estimates generated using statistical models. Even under such circumstances, Japan was regarded as having the best health-care system in the world.
Nearly 20 years later, in 2017, a research team of which I was a member published an article in the British medical journal The Lancet that analyzed changes in healthy life expectancy in Japan by prefecture. The MHLW had published a report in 2013 that laid out two major goals: increasing healthy life expectancy and decreasing disparities for this expectancy among the country’s 47 prefectures. Our analysis revealed that while healthy life expectancy was increasing overall, gaps among prefectures had grown more pronounced between 1990 and 2015 (Figure 3). There was a 2.7-year difference in healthy life expectancy between the highest-ranking prefecture, Shiga, and the lowest ranking one, Aomori. This gap suggests there is a real difference in mortality rates and the prevalence of disability between these two prefectures. Moreover, as shown in Figure 4, the rate of decline in the age-standardized mortality rate, which corresponds to the level of improvement in health, has stagnated in recent years. This stands in direct contradiction to the stated goals of the 2013 MHLW report.
Figure 3. Estimated Life Expectancy and Healthy Life Expectancy by Prefecture in 2015
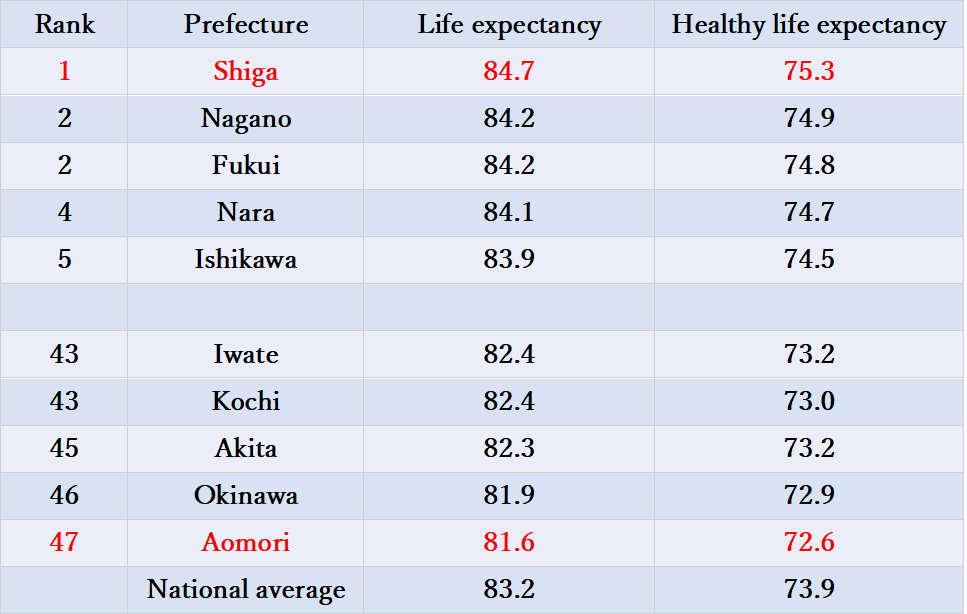
Source: Nomura et al., “Population Health and Regional Variations of Disease Burden in Japan, 1990–2015: A Systematic Subnational Analysis for the Global Burden of Disease Study 2015,” The Lancet 2017.
Figure 4. Change in the Age-Standardized Mortality Rate from 1990 to 2015
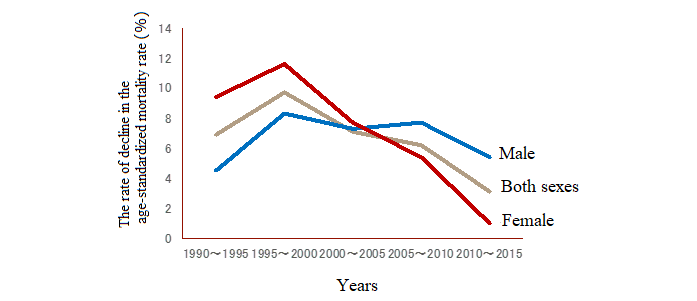
Source: Nomura et al., “Population Health and Regional Variations of Disease Burden in Japan, 1990–2015: A Systematic Subnational Analysis for the Global Burden of Disease Study 2015,” The Lancet, 2017.
As improvements in health indicators stagnate and disparities in health outcomes grow wider, another concerning problem has gone largely unnoticed. Doctors, nurses, and other health professionals are overworked to the point that maintaining current standards is becoming unsustainable. The stereotyped image of a career in medicine being an attractive and well-paying profession is a thing of the past. The health-care sector is now among the toughest and most demanding of professions—a transformation that was underway well before the pandemic. That the pandemic brought the health-care system to the verge of collapse should come as no surprise. Data presented to the MHLW committee to review work-style reforms in the medical sector, of which I served as vice-chairperson, indicated that average monthly overtime for physicians far exceeded the 80-hour limit stipulated by the Labor Standards Act and the annual total of 960 hours established by the Shinzo Abe administration. Younger physicians working at hospitals put in particularly long hours, their overtime sometimes exceeding 2,000 hours per year.
Epitomizing this problem is the plight of “unpaid doctors”—tuition-paying, graduate medical students who are ostensibly undergoing training at university hospitals in hopes of landing a coveted post there. They have little time for research, however, since they are seeing patients all day, and they need to work part-time over the weekend to make ends meet. Most people in Japan do not realize that the high acclaim accorded to the country’s health-care system rests on their sacrifices.
In the hope of shedding light on their dilemma, I included a sentence at the beginning of the MHLW work-style reforms committee’s interim report that read, “We must first acknowledge that our health-care system is in a state of crisis and is being sustained largely by the self-sacrificing work of medical practitioners who put in extremely long hours.” I was greatly surprised at how much pushback I received for this simple statement. It was only after running a media campaign to improve young doctors’ working conditions at university and acute-care hospitals that the Ministry of Education, Culture, Sports, Science, and Technology began studying the issue of unpaid doctors and that improvements were made to rectify these structural failures.
Nevertheless, the fact remains that many hospital physicians continue to be overworked, and the root of the problem is Japan’s inefficient health-care delivery system. There is a lack of differentiation, stemming from an overabundance of small and midsize private hospitals, all seeking to offer a full range of services. This system is well-suited to meeting basic needs, to be sure, but is woefully inadequate during times of emergency, as was made all too clear during the COVID-19 pandemic. Even more problematic is that many young physicians are without institutional protection regarding medical errors. Accidents are bound to happen, no matter how much care is taken. Many malpractice verdicts in Japan, though, identify young doctors as the cause of injury, often noting that they were “unskilled,” “inexperienced,” or “careless.”
Heaping blame on overworked, underpaid young doctors will do nothing to prevent errors or guarantee patient safety. And mounting pressure to cut medical expenditures only adds to the sense of exhaustion. A step in the right direction might be to protect such workers with a no-fault compensation system that is not funded with insurance premiums or taxes, as proposed by Giichiro Oiso, professor at the Hamamatsu University School of Medicine.
While working at the WHO, I had the good fortune to befriend Swedish Professor of International Health Hans Rosling (1948–2017), well-known in Japan for his bestseller Factfullness. He was a physician who actively promoted the use of data and data visualization, which he used to communicate effectively with the public. He is known to have remarked, “Health cannot be bought at the supermarket. You have to invest in health.” This is an important point to keep in mind at a time when attempts to slash medical expenditures could wind up devastating our health-care system.
Heightened Sense of Insecurity
The degree to which people have been affected by COVID-19 varies greatly depending on where they live and work, and this has laid bare the many socioeconomic disparities around us. We live at a difficult time when local governments, companies, and even individuals must take steps on their own to manage and protect against risks—a trend seen not just in Japan but worldwide. Even before the pandemic, the sense of insecurity felt by people around the world was on the rise, according to the most recent report from the United Nations Development Program. Even in wealthy countries with strong economies and high health indicators, only 23% said they feel secure; the rest report some level of insecurity (Figure 5). The share of people harboring insecurity has no doubt risen since the outbreak of the pandemic, the start of war in Ukraine, and recent examples of the consequences of climate change.
Figure 5. Many People Feel Insecure Even in High Human Development Index Countries
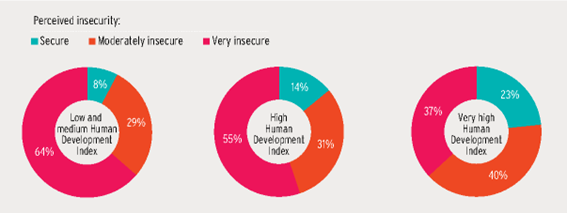
Source: Human Development Report Office, “World Values Survey.”
Why is the feeling of insecurity growing? A UNDP report looks at this question from the standpoint of human security and argues that the increase is chiefly due to new types of threats that are beyond the scope of personal protection and empowerment. As exemplified by COVID-19, the Russian invasion of Ukraine, growing economic disparities, and the adverse impact of digitalization, these threats are often intertwined and are global in scale. Addressing threats to human security requires not only protection and empowerment but also greater solidarity among individuals and communities across national borders. The UNDP calls for developing trust as a key component connecting the three elements of protection, empowerment, and solidarity.
This is not just an empty hypothesis. A paper published by an international team of researchers in The Lancet, to which I also contributed, empirically demonstrates the importance of trust. By analyzing the number of COVID-19 cases and deaths in 177 countries between January 2020 and September 2021, the paper identified the factors that had the biggest impact in coping with the pandemic. Population density, obesity, per capita GDP, and seasonality were all factors that were statistically significant in the number of cases and deaths. But they were not able to explain the differences seen among countries. Pandemic readiness indicators were statistically irrelevant. Surprisingly, of far greater significance in both reported numbers and vaccination rates was trust in one’s government and in other people.
Transitioning to an Autonomous, Decentralized, and Cooperative System

Trust is a foundational element in building a socioeconomic system, and health care is no exception. We are currently witnessing a transition to Web 3.0, the latest iteration of the World Wide Web. As shown in Figure 6, Web 1.0 was a world of one-way communication, comprising search engines and e-commerce accessed from a personal computer. The present, however, is dominated by Web 2.0, which is characterized by two-way, interactive communication, the dominance of Big Tech, and the ubiquity of smart phones. Web 3.0 will likely be more autonomous and decentralized, incorporating artificial intelligence and blockchain technology. Trust in the world of Web 2.0 is secured by major platforms like Amazon, but Web 3.0 promises to enable users to secure trust at the individual level.
Figure 6. The Evolution of the World Wide Web
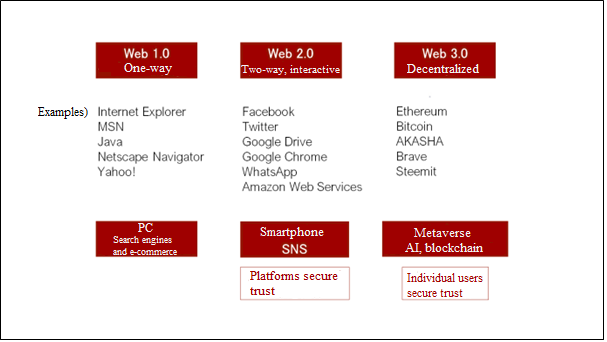
The state of health-care today most closely resembles Web 1.0, as patients normally have little choice but to submit to the instructions given by their care provider. This is not to say, though, that people would find themselves more empowered were the health-care system to evolve to Web 2.0. A pertinent example of the abuses of social media was former British Prime Minister Boris Johnson’s push for Brexit. His chief adviser, Dominic Cummings, analyzed data from the social media posts of British citizens and found that those who do not vote generally felt they had little control over their lives. He used this finding to come up with the slogan “Let’s Take Back Control,” adding the spin that the encroaching hand of Brussels posed a threat to the British way of life.
Web 2.0 has enabled private individuals to publish and broadcast their ideas to a much wider audience, but the irony is that this has not led to empowerment; if anything, the platforms have been the beneficiaries as they profit from the utilization of this data to divide and manipulate individual users.
As we now head toward Web 3.0, the health-care sector needs to grapple with the question of how to ensure the trustworthiness of its services and enable people to take control of their own health. Even if the application of such technologies as virtual reality and augmented reality is still years away, the autonomous and decentralized aspects of Web 3.0 are already becoming a reality in this sector. Let me cite two examples.
The first is the use of the SMART Health Card (SHC) as a digital vaccine certificate. Canada, Singapore, and the United States have adopted a system of democratized mutual trust with the SHC that resembles academic peer reviews. This stands in stark contrast to China and the European Union, where the state guarantees trust. SHC data is held in a decentralized manner in each individual’s smartphone, and it is the individual who retains control over data access. This is an approach to data protection that aligns with values of a democratic society.
Figure 7. Developing International Standards for Digital Vaccine Certification
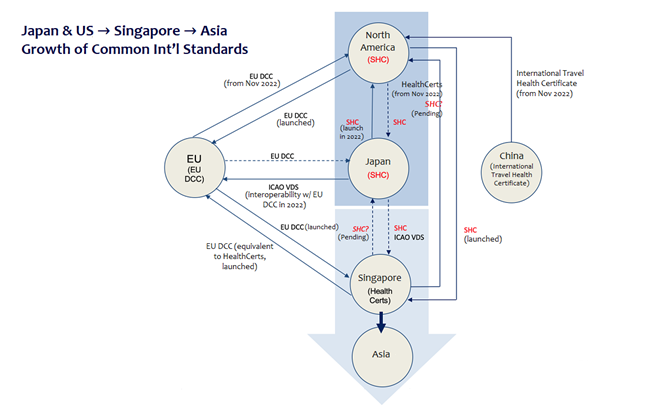
Notes: Straight lines indicate standards already in use or are scheduled for implementation. Dotted lines indicate those that should be considered. Application in the EU may differ according to member state.
Source: The Commons Project.
Japan, in principle, likewise employs the SHC system, entrusting data management to the individual. There is no need for approval from the government or a certifying organization. The choice of such an autonomous, decentralized is quite remarkable, given Japan’s propensity to rely on authority, and credit for this decision should go to the Digital Agency. The digital vaccine certificate could serve as a model for a personal health record mechanism that allows patients to keep and manage their personal health information. Such technology would help clear the longstanding challenges to achieving a standard format for electronic medical records and enable a transition to an autonomous and decentralized health-care system.
The second example is the COVID vaccination effort in the city of Soma in Fukushima Prefecture. As director of the Soma COVID-19 Vaccination Medical Center, I have been supporting the vaccination programs in Soma and Minami Soma. These two cities were the first in the country to complete administering four doses of the vaccine and were only minimally affected by the seventh wave of infections in Japan. There are several reasons for the success of the “Soma model.” First, it was decentralized. Rather than having the cities’ residents make appointments on their own, dates and times were allotted to each neighborhood, with appointments being chosen by a lottery to ensure fairness.
Administering vaccines on a neighborhood basis fostered a sense of community. Residents receiving doses at around the same time were able to share experiences, including those of side effects, heightening their sense of responsibility for protecting each other’s health and encouraging more people to voluntarily seek out vaccinations. The vaccination rate for middle and high school students was particularly notable. The project was bolstered by the feeling of solidarity among residents, city officials, and medical professionals that had formed organically in the wake of the 2011 Tohoku earthquake and tsunami. In addition, Soma shared detailed information about possible side effects on the city’s website in an attempt to enhance transparency, and this had the effect of increasing public trust in vaccination.
Decentralized, autonomous organizations are a prominent feature of Web 3.0. In his 2018 The Square and the Tower, author Niall Ferguson notes how, throughout human history, hierarchical organizations and decentralized networks have at once competed against one another and maintained a mutually complementary relationship. He argues that the period from the 1970s to the present marks only the second time in history when decentralized networks have predominated (the first being the late-fifteenth to late-eighteenth centuries). Moving forward, the importance of decentralization for our social, economic, and health-care systems will grow, and my focus at the Tokyo Foundation for Policy Research will be on analyzing autonomous, decentralized, and cooperative systems and publishing proposals for such organizations in the health-care sector.